Many families wait too long to have the hospice conversation. They hear the word hospice and think it means giving up hope – or that it’s only for when someone has just days to live.
Other patients are referred so late that they pass away within hours or days of enrollment, never getting the full benefit of hospice services. As a result, patients and loved ones miss the support, guidance, and relief they deserve.
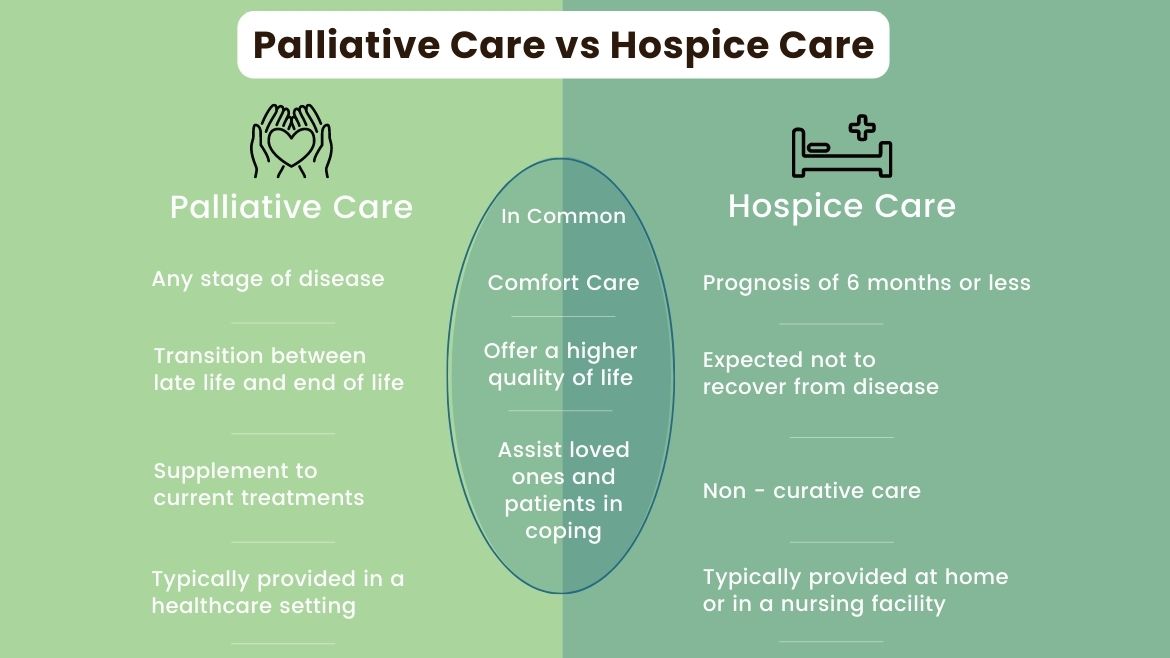
Hospice is a team‑based service that shifts the goal from curing an illness to maximizing comfort and quality of life in its final stage. Care can happen at home, in a nursing facility or in an inpatient unit.
Contrary to a popular myth, hospice does not speed up death. In fact, several studies show the opposite is true. One study of patients with advanced heart failure found that those in hospice had longer median survival compared to those receiving standard care (80 days vs. 71 days). With hospice, families also gain 24/7 on-call nursing support, counseling, and help navigating insurance and medical supplies – resources that are hard to assemble on their own.
How do you know if hospice is what your loved one needs at this time? Overall, doctors must determine that a patient is likely to have six months or less to live if the illness follows its usual course. Prognosis isn’t an exact science, but these signs often signal it’s time to have the hospice talk:
-
Major decline in day‑to‑day function
If someone who once drove, cooked and bathed independently now needs help dressing or walking to the bathroom, pay attention. Rapid loss of independence indicates a disease is advancing.
-
Unintentional weight loss
Dropping about 10 percent of body weight in six months – even while eating – suggests the body is struggling to use nutrients.
-
Frequent hospital or emergency room visits
Repeated admissions for the same problem (such as heart failure flare-ups, COPD exacerbations, infections) usually mean the condition is no longer controlled by standard treatment.
-
Worsening symptoms at rest
Shortness of breath while sitting, pain that no longer responds to current doses, or extreme fatigue can all point to late-stage illness.
-
A year-ahead question
“Would I be surprised if this patient died within the next year?” If the answer is, “no,” hospice deserves serious consideration.
 It’s never easy to think about end-of-life care, but waiting too long can mean missing out on valuable support, comfort and connection. If your loved one is declining, has been in and out of the hospital, or no longer has the strength for once-routine activities, it may be time to open the conversation.
It’s never easy to think about end-of-life care, but waiting too long can mean missing out on valuable support, comfort and connection. If your loved one is declining, has been in and out of the hospital, or no longer has the strength for once-routine activities, it may be time to open the conversation.
Maybe it isn’t time for hospice; perhaps palliative care is more appropriate. CHP also provides this care option that focuses on patient comfort, a higher quality of life, and assistance for family members.
Talk openly with your doctor or health providers. Ask questions, share concerns and most of all, don’t wait.
You’re always welcome to contact your local, nonprofit, CHP Home Care & Hospice office. Our friendly, helpful staff can help answer questions and even provide an initial assessment to help you make an informed decision.
###

